Pupillometry is the measurement of the size and dilation of a person’s pupils. This measurement is then converted into information that can help diagnose many different neurological problems. When a person is under heightened mental or physical stimulation, their pupils will dilate.
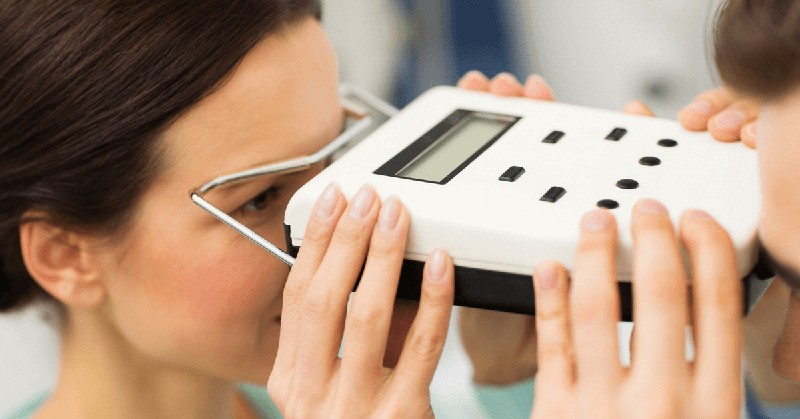
Nowadays, doctors can use this technology in a neuro exam. The pupilometer is the device used in pupillometry. This tool helps them look at the eye’s pupil size, constriction rate, and reaction time. By interpreting these parameters, they can determine if there’s something wrong with the patient’s brain.
In this article, we’ll be looking at the pupilometer and its relevance to diagnosing neurological diseases.
What is a pupillary response?
The pupillary response is the measurement that results from the pupil’s interaction with signals from the brain. When the brain sends a message to the eye, the pupil will dilate or constrict. A healthy pupil has a diameter of about 2-4 millimeters, which is about the size of a pencil point. The pupil will constrict to about 1 millimeter in diameter in response to a stimulus.
But dilation or constriction is not a one-way street. The eye will also send messages to the brain. These signals will then determine the speed and accuracy of the pupil’s response.
How does the pupillary response help doctors diagnose neurological problems?
The pupillary response is one of the tests doctors use to evaluate patients with neurological problems, such as brain tumors and multiple sclerosis. The presence or absence of a response can help us confirm the presence of certain diseases and determine the severity of a problem.
The degree of dilation or constriction can give doctors a clue to the cause and extent of a problem. The most common pupillary response is an abnormal constriction.
What is the role of the pupilometer in detecting neurological problems?
The pupilometer can detect changes in the pupillary response and constriction velocity by measuring how much light goes through the pupil. By comparing the normal response with the response during neurological tests, we get more information about the cause and extent of a problem.
The pupilometer is a simple, non-invasive way to measure the pupil’s response to light for the early detection of neurological problems.
Two of the most important neurologic exams
Neurologic exams are a series of tests to evaluate the nervous system. Tests assess how each part of the nervous system is functioning. In a complete exam, all of the parts of the nervous system are evaluated.
The pupilometer can be used with a neurologic exam conducted by a doctor, nurse, or trained therapist. The various neurologic exams include
1. The five-step exam
The five-step exam is a neurologic screening test for any disease or condition that affects the central nervous system. It checks for mental status, cranial nerves, motor strength, and coordination.
Mental status: All four areas of mental status are evaluated, including the patient’s level of consciousness, mood and behavior, speech, and ability to reason and concentrate.
Cranial nerve testing: 12 cranial nerves are tested. These include the eyes, ears, nose, mouth, and throat (cranial nerves I-XII).
- CN I: In cases when a frontal tumor is suspected, such as in Foster-Kennedy syndrome, where one optic nerve is pale owing to compression and edema of the contralateral nerve due to elevated intracranial pressure, the contralateral optic nerve is not checked for this nerve.
- CN II: This afferent nerve is tested during visual acuity, color vision, and pupil testing using the swinging lamp test for afferent pupillary deficiency and visual field testing.
- CN III: Extraocular motility is a standard method of testing for this. Four of the six extraocular muscles, including the levator palpebrae superioris (which lifts the top eyelid), are innervated by this nerve, which is responsible for elevating, depressing, and adducting the eye. Pupillary constriction is another effect it has. An aneurysm is more likely to develop a pupil-involved CN III palsy because pupillary fibers travel on the outside of the nerve and are susceptible to compression.
- CN IV: Extraocular motility is a common method of testing for this. The superior oblique muscle, which is responsible for both torsion and depression of the adducted eye, receives its supply from this nerve. An ipsilateral head tilt and contralateral gaze show a hyper deviation in numerous gaze regions.
- CN V: CN III, IV, and/or VI dysfunctions may suggest a cavernous sinus lesion if there is decreased feeling in the V1 and V2 distributions.
- CN V: The lateral rectus muscle, which is responsible for abducting the eye, is innervated by CN VI, often evaluated for extraocular motility. In circumstances of elevated intracranial pressure, there may be a decrease in the ability to abduct.
- CN VII: An abduction deficiency may indicate an imbalance in facial asymmetry. A neurological injury in the cerebrum is characterized by an upper motor neuron lesion. A lower motor neuron will affect the bottom part of the face.
- CN VIII: Abduction deficits need hearing tests since the cerebellopontine angle is adjacent to the cranial nerves VI, VII, and VIII. Having a patient with unilateral hearing loss and an abduction deficit might point to the presence of a benign tumor-like an acoustic neuroma.
- CN IX and CN X: Since their anatomical proximity makes it difficult to find discrete lesions, they aren’t examined independently. Dysphonia, dysphagia, and dyspnoea are all signs of nerve or structural dysfunction. Patients with diplopia, ptosis, or both may have myasthenia gravis, and CN IX and X should be examined for signs of neuromuscular junction dysfunction.
- CN XI: The sternocleidomastoid muscle is mostly unaffected by upper motor neuron injuries, whereas the trapezius muscle is more severely affected. In situations of suspected myasthenia gravis, this is a crucial test.
- CN XII: A lower motor neuron injury causes the tongue to shift to the ipsilateral side, whereas an upper motor neuron lesion causes it to shift to the contralateral side. Tongue atrophy is an indication of lower motor neuron damage.
Conclusion
Medical doctors increasingly use pupillometry to gather information about patients by measuring their eyes. By using the NPi pupillometer, doctors can accurately diagnose neurological problems and other common diseases that had previously been difficult to identify.




More Stories
How to Choose Physio Napier | 6 Things to Consider
Health Hygiene to Avoid Flu
Am I working out too much?